·
NAME:G.JAGADEESH
o ROLL
NO:37
Second year
MBBS[3RDsem]
BATCH:2019
QUESTION-1
1)NEUROLOGY
A) https://143vibhahegde.blogspot.com/2021/05/wernickes-encephalopathy.html
A 40 year old
male presented to the hospital with a chief complaint of irrelevant talking and
decreased food intake since 9 days
Who is from
YADAGIRIGUTTA
The patient
was asymptomatic since 9 days.he suddenly started talking and laughing at
himself,which is also associated with decreased food intake.he also had a short
term memory since9days and gave a complaint that he was not able to recognize his
family members from time to time.
He also had a
2-3 episodes of seizures
He was also
suffering from type 2 diabetes since 2 years and no history of hypertension.
He takes a
normal mixed diet and actually apetite was decraesedand disturbed sleep.bowel
movements were regular.
Moreover he
was addicted to alcohol and cigarette and has no habit of chewing tobacco.
No similar
complaints in his family.
Upon general examination he was conscious
,cooperative but not coherent.alcohol inhibits the action of vit B1 which leads
to wernicke’korsakoff syndrome
Actually thiamine is necessary of optimal
metabolism of carbohydrates because THIAMINE PYROPHOSPHATE s the coenzyme for
many enzymes in CARBOHYDRATE METABOLISM.
Due to chronic alcoholism there is accumulation
of more amount of acetic acid andalso lactic acid due to anaerobic respiration
Chronic alcoholism also reduces the absorption of
THIAMINE fron INTESTINES .
Which lead to deficiency of THIAMINE which lead
to wernicke’s Korsakoff syndrome.
This disorder leads to
OPTHALAMOPLEGIA
ENCEPHALOPATHY
NYSTAGMUS
CEREBELLAR ATAXIA
FINALLY MAY ALSO LEAD TO POLYNEURITIS.

On examination he was found to be absent of
pallor,icterus,cyanosis,clubbing,lymphaedenopathy.
Investigations
done are chest Xray,ECG,CBP,urine levels
of ch loride,sodium potassium.
And ketone bodies are absent.LFT AND RFT also performed.he also reffered to
pshychiatry and surgery.the provisional diagnosis was wernicke’s
encephalopathy.The diagnosis was good and iam satisified with
the treatement.
2)GIT
ACUTE
PANCREATITIS
https://caseopinionsbyrollno05.blogspot.com
A
29 year old patient presented to hospital with developing abdominal pain and
also vomitings which was suddn in onset .
He
is actually a known case of pancreatitis and also a known case of diabetes
mellitus type 2.HT,asthma,TB and epilepsy.
His
diet was normal mixed diet with apetite decreased,regular bowels andbladder.
Micturition
was normal.he is an alcohol addict.
No
similar family history.
On
general examination patient was found to be concious ,coherent and
cooperative.there was no pallor,icterus,cyanosis,clubbing,lymphaedenopathy and
pedal edema.
Vitals
were normal.
Tenderness
observed on deep palpation in abdomen.
They
have done ultrasound abdomen to him.
The
diagnosis and treatment is satisifactory.
3)PULMONOLOGY
https://divyaraju266.blogspot.com/
A55
tear old femalepresented with chief complaints of shortness of breath,pedal
oedema and puffiness of face.
Her
shortness of breath was of grade 4 and it is probably due to COPD-bronchietasis.
Vitals
of her were normal.
The
treatement was satisifactory and nice the list of drugs is large but they are
important.
4)
CEREBELLAR ATAXIA
https://kausalyavarma.blogspot.com/
A52 year old male presented with giddiness
associated with one episode of vomitingTthere is a lesion in cerebellum.There
is presence of infarct in inferior cerebellar hemisphere of the brain.
Symptoms are loss of muscle control or
coordination of voluntary movements such as walking and picking up of
objects.INTENTIONAL TREMORS.
There is deprived of nutrients and oxygen to
the brain .the treatement was good.
Investigations
done are CT scan ,LFT ,RFT ,CUE.
5) CVS
A 45 year
old female presented with palpitation , radiating chest pain along left upper
limb and pedal edema.
Past reports:
*(right and left)paresis due to hypokalemia 1year
back
2 months back came to KIMS NARKETPALLY for
treatment of neck pain for which she received medication:
She
has a normal mixed type of diet.apetite was normaland bowel movements were
irregular.vitals were normal.edema is pitting type of edema.
Investigations
done are CBP ,CUE ,RFT ,CHEST X-RAY ,CRETININE LEVEL..treatement is nice.
6)HEART
FAILURE WITH DIABETES
https://muskaangoyal.blogspot.com/
A 73 old male
presented with pedal edema ,shortness of breath ,decreased urine output.
He is a
chronic alcoholic and has pedal edema since 4 years , blurring of vision since
4 years.Decreased urine output since 2 days.
The diet he
was taking is of normal mixed diet ,apetite was normal ,normal bowel movements
but there is decreased urine output.
On general
examination he was said to be pallor and pedal edema but no icterus ,cyanosis
,clubbing ,lymphadenopathy.
He is
heavily built with central truncal obesity and a ulcer on left limb.vitals were
abnormal
Both heart sounds were heard normal and found to be normal
no any additional murmurs.shape of abdomen was distended and tenderness absent.
INVESTIGATIONS done are
CBP ,LFT ,ABG ,X-RAY CHEST ,ECG.Treatement is
satisifactory.
7)BILATERAL THROMBUS.
https://preityarlagadda.blogspot.com/
A 52 year old male came to the OPD
with chief complaints of decreased urine output and shortness of
breath.shortness of breath was of grade 2.
Apetite was normal diet is of
mixed type ther eis history of constipation and bladder movements were
normal.On examination he was conscious
,coherent ,cooperative.
Vitals were normal.Both sounds of
the heart are heard normally and no murmurs.
Investigations
done are CBP,ALBUMIN ESTIMATION ,RFT ,BLOOD UREA LEVEL ,SERUM CREATININE ,ABG
ANALYSIS ,LFT ,CT PULMONARY ANGIOGRAM.
The
doctor was good and given many good advices to the patient on diacharge and treatement
was good.
8)ACUTE
PANCREATITIS WITH DENOVO DIABETES
https://nehae-logs.blogspot.com/
A 25 year old man presented with abdominal
pain , an episode of vomiting and shortness of breath.dyspnoea is of grade
3.there was no similar complaints in the past.diet is of normal mixed type
apetite was normal regular bowel and bladder sleep is reduced due to pain.
On general
examination he was conscious ,coherent ,cooperative.there was no pallor
,cyanosis ,icterus ,clubbing ,pedal edema ,no lymphadenopathy no generalised
anasarca
Vital were
abnormal and some what elevated
In systemic
examination there is found to be tenderness around umbilical and epigastric
regions.
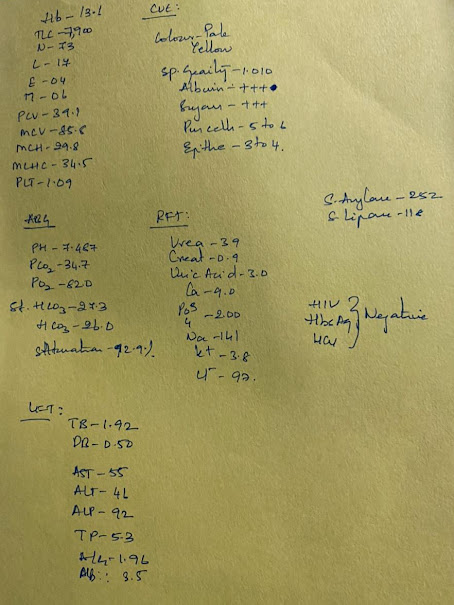
INVESTIGATIONS
done are CBP ,CUE ,ABG ,LFT ,RFT.
There is
albumin and sugar in urine serum amylase levels are elevated and also serum
lipase levels are also elevated
OTHER
INVESTIGATIONS DONE ARE X-RAY CHEST ,ULTRASOUND ABDOMEN.
Altered head
of pancreas
Fatty liver
at grade 1
Minimal ascites
ECG also
done.
Diagnosis is
acute pancreatitis and acute cholecystitis with donovo diabetes type 2.
Plan and
action of treatement were satisifactory and list of drugs is long.
9)NEPHROLOGY
https://drsaranyaroshni.blogspot.com/
A 8 year old
boy presented with frequent urination.
His mother
have noticed that her son urinates almost 25 times a day.
There is no
associated flank pain ,abdominal pain ,burning sensation while micturition.
There is no
history of fever ,malaise.
He weighted
19kg and height 127cm he has 0 episodes on bed wetting.
there
is also history of constipation and have been almost resolved by diet modification.
INVESTIGATIONS
done are
Urine
examination
Urine
culture and sensitivity report
Serum
electrolytes
There
is no nocturnal enuresis.
There
is no treatement given.
10)LIVER
ABCESS
https://kavyasamudrala.blogspot.com/
A 58 year
old male patient who is a palm tree climber by his profession presented with
Pain abdomen
,decreased apetite and fever since 2 days.
He
had developed pain in right upper quqdrant of abdomen it is dragging type ,nonradiating ,and sudden in onset.
Diet
is of normal mixed type , apetite is decreased ,bladder and bowel movements are
normal ,sleep is adequate.
He
is an chronic alcohol addict.
Upon
General examination he was found to be conscious ,coherent .
,cooperative.moderately
built and nourished.
Vitals
were normal.
Pallor
is present but no signs of icterus ,cyanosis ,clubbing ,lymphadenopathy ,edema.
Abdomen
is slite tender and soft
Both
sounds of heart were heard and found to be normal without any murmurs.
INVESTIGATIONS
ARE
BACTERIAL
CULTURE
X-RAY
CHEST
CBP
LFT
RFT
The
treatement was good and follow up was given to this patient.
QUESTION-2
I
have still not made any blog to upload in this.i did not get any chance till
now.
QUESTION-3&4
CVS
:
https://60shirisha.blogspot.com/
This
is a case of heart failure.due to left ventricular dysfunction
A
70 year old patient presented withdistended abdomen and shortness of breath.
She
is a hypothyroid patient since 5 years.so she was on thyronorm 100mg .
Her
apetite was normal with diet mixed regular bowel and bladder movements sleep is
also adequate.
There
is slight variation in temperature all other vitals are normal.
Syatemic
examination is also done accordingly.
INVESTIGATION
done are done
ECG
DONE AND SHOWN ATRIAL FIBRILLATION
CBP
SERUM
ELECTROLYTES
HbA1c
CRP
PROTIEN
RANDOM
BLOOD SUGAR
BLOOD
UREA LEVEL
Treatement
plan is also nice but they failed to control the thyroid levels in this patient
if they have done so she would have not passed away during defibrillation.
I don’t
have idea about wether she has continued her thyronorm daily or not and they
have not mentioned in this case sheet also.
If
she have used thyronorm I think she would have not passed away.
QUESTION-5
Every
week we will get postings for 2 days in this pandemic.the theory classes are
going on very well.
But
we are not understanding anything in our postings because audio is not clear
that we cant here them .
Till
now we have learnt some thing about general examination .
And
GIT classes are going on and also diseases associated with it.
And
we are also learning history taking.


















Comments
Post a Comment