60 year old male carpenter
This is an online e log book to discuss our patient de-identified health data shared after taking his/her/guardians signed informed consent. Here we discuss our individual patient problem through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evidence input.
This E blog also reflect my patient centered online learning portfolia and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempts to understand the topic of patient clinical data analysis to develop my compentency in reading and comphrending clinical data including history , clinical finding , investigation and come up with diagnosis and treatment plan....
A 60yr old male Carpenter by occupation came with the complaints of:-
1. Enlarged stomach since 1 month
2. Fluid retention in legs since 1 month.
(Both complaints started at the same time)
History of presenting illness-
The patient was apparently alright 1 month back then he noticed enlargement of his stomach which is insidious in onset, gradually progressive, and relieved on abstaining from alcohol and it is associated with squeezing type of pain in the umbilical region which is aggravated on eating food and working and relived on taking medications.
H/O B/L PEDAL EDEMA - Pitting type extending upto knee level.
H/O Intermittent Fever - low grade,associated with chills and rigors and releived by medication.
No H/O nausea, vomiting,weight loss, hematemesis, melena.
History of Past illness-
Patient has similar complaints in the past of jaundice 10 years back for which he relieved by treatment.
The patient has history of 1 seizure episode 10 years ago.
The patient has history of hypertension and diabetes mellitus since 7-8 years and is on medications.
N/K/C/O - TB, Asthma, CVA, CAD, Thyroid disorders.
Personal history-
Daily routine-
Diet- initially mixed diet but switched to vegetarian diet after seizure episode.
Appetite- decreased since 1 month
bowel movements- constipation since 1 month (Passing stools once in 2-3 days)
Bladder movements- burning micturition and decreased urine output. increased urination on medications.
Addictions- smoker and alcohol consumption for at least 40 years.
Family history-
History of diabetes mellitus in patients mother.
General examination-
I have taken consent for examination and examined the patient in a well light room-
The patient is conscious, coherent, cooperative and oriented to time place and person.
The patient is Well built and nourished.
Pallor- present
Pedal Edema - Bilateral pedal Edema
Present Pitting type
No signs of Icterus,Clubbing, Cyanosis,
Lymphadenopathy
Vitals-
TEMP: Afebrile
BP: 140/70mmHg
PR: 102 bpm
RR- 24cpm
Spo2- 96% @RA
GRBS:485mg/dL
Systemic Examination:
PER ABDOMEN
On inspection:
Abdominal distention - Present
Abdominl Girth-85cms
All quadrants are moving equally with respiration
Umbilicus - central and inverted
Engorged Veins present but not around umbilicus
No scars, prominent Venous pulsations and visible peristalsis.
On palpation:
There is no local rise of temperature or tenderness.
Liver- non palpable
Spleen- non palpable
No guarding, rigidity
On percussion:
Shifting Dullness present
Fluid thrill- absent
On auscultation:
Bowel sounds heard
CVS:
On Inspection:-
Chest wall is bilaterally symmetrical.
No precordial bulge is seen
On Palpation:-
JVP- Normal
Apex beat -felt in the left 5th intercoastal space in the mid clavicular line
Auscaltation-
S1&S2 are heard,no murmur found.
RESPIRATORY SYSTEM
Position of trachea- central
Bilateral air entry, normal vesicular breath sounds are heard.
No added sounds
CNS
Patient is conscious ,coherent and co operative well oriented to time and space.
Speech normal.
No signs of meningeal irritation.
Motor and sensory system- Normal
Reflexes - present
Cranial nerves - intact
Provisional Diagnosis-
Chronic liver disease with Portal Hypertension and Anemia.
INVESTIGATIONS:-
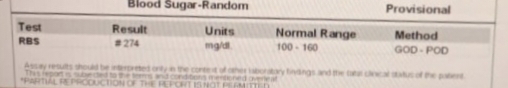
Random Blood Sugar (RBS)
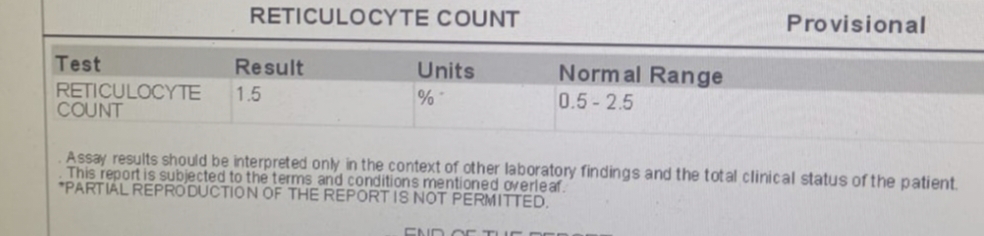
Reticulocyte count:-
Prothrombin time:-
Serology:-
Ascitic fluid for LDH and SAAG:-
Ascitic Tap done on 8/07/2023 -1L of ascitic fluid collected.
RFT:-
sr.electrolytes:-
Urine for Ketonebodies:-
CUE:-
ECG:-
2dEcho:-
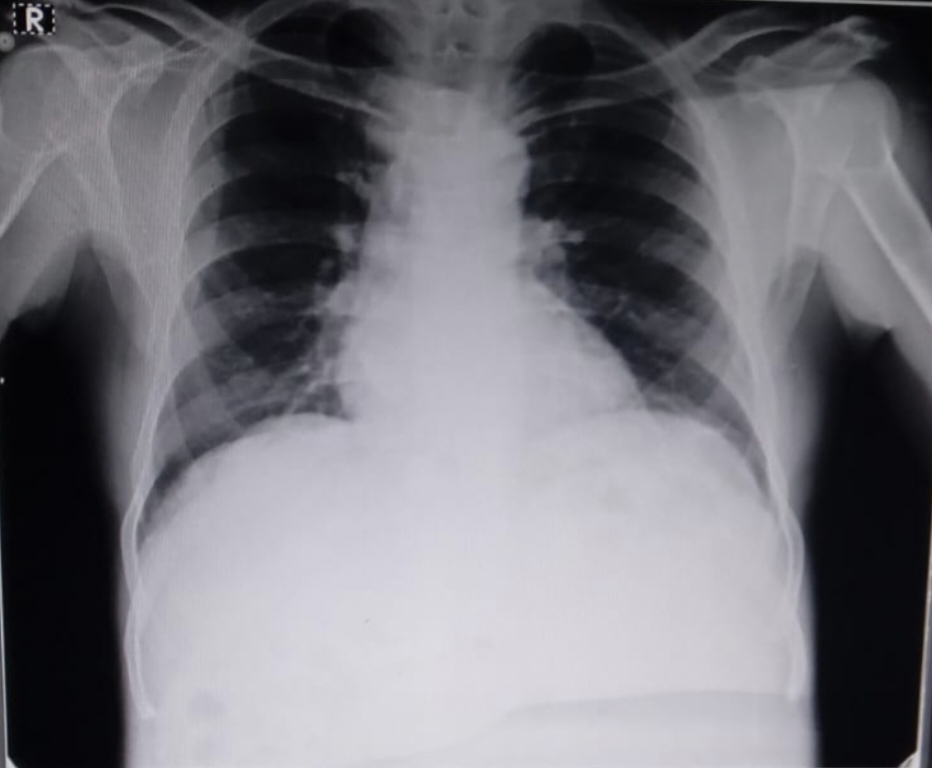
Chest X-Ray PA-View:-
USG-Abdomen:-
Treatment-
1.Inj- HAI 6units IV/STAT
2.Inj.HAI SC/TID
3.Tab.LASIX 40mg PO/BD
4.Tab.PCM 650mg PO/OD
5. GRBS monitoring .































Comments
Post a Comment